What is Metabolic Syndrome?
Metabolic syndrome is a bundle of cardiometabolic risk factors that develop in common genetic and environmental environments, characterized by large waist circumference, high blood pressure, qualitative and quantitative disorders in blood lipids, and high blood sugar. People with metabolic syndrome are 5 times more likely to develop type 2 diabetes and 2 times more likely to develop atherosclerotic cardiovascular disease than those without metabolic syndrome.
To be diagnosed with metabolic syndrome, at least three metabolic risk factors must be present.
Table 1: Definition of metabolic syndrome

The surgical treatment of Metabolic Syndrome is called Metabolic Surgery.
In the last half of the 20th century, experiments were conducted to see if diseases such as high lipids and cholesterol could be treated with surgical operations such as intestinal bypass.
In 1995, Dr. Walter Pories and his research team published a paper suggesting that "Diabetes in adults can be treated surgically." This article was a turning point. In the following years, it was found that Type 2 diabetes and metabolic disease could be treated surgically.
In 2009, "American Bariatric Surgery Association" changed its name to "American Metabolic and Bariatric Surgery Association", taking into account the beneficial effects of surgical methods, especially in the treatment of Type 2 Diabetes Mellitus and metabolic syndrome.
Today, the term Metabolic Surgery is used specifically to describe procedures to treat type 2 diabetes and metabolic diseases.
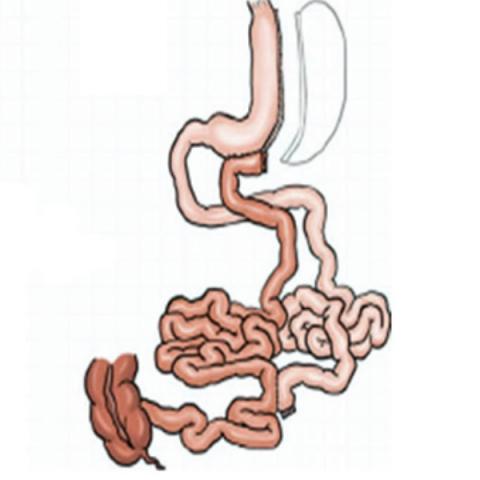
Ileal Interposition
The term ileal interposition is the process of replacing the last part of the small intestine with the initial part. This surgery works on the principle of deactivating the hormones that cause insulin resistance and raising the hormone levels that increase insulin sensitivity.
Ileal Interposition operation is a surgical treatment method developed for the treatment of Type 2 Diabetes since the beginning. The definition of metabolic syndrome includes Type 2 Diabetes, hypertension, high cholesterol and triglyceride levels, and overweight.
Ileal Interposition surgery is not an obesity surgery as a starting point. It is an operation that aims to treat all health problems within the scope of Metabolic Syndrome, especially Type 2 Diabetes. Therefore, obesity is not among the criteria for ileal interposition surgery.
Ileal Interposition surgery does not cause absorption restriction or malabsorption. Patients who have had ileal interposition surgery start to consume liquid food on the 3rd day after the surgery. Within six months to 1 year, they can survive with a completely free diet and without vitamin or mineral supplements.
Patients who are fit for surgery usually stop all diabetes, blood pressure and cholesterol medications they use after Ileal Interposition surgery. They are observed in terms of the course of these diseases during the hospitalization period after the surgery. The vast majority of patients are discharged without using any of these drugs. In some of them, until the metabolic effect settles, the use of drugs continue at gradually decreasing doses for periods ranging from a few weeks to a few months, in a controlled manner. When the measurements return to normal, the use of all of these drugs are stopped.
The effect of weight loss is not much due to the partially wider tube stomach, so it is beneficial for patients who do not want to lose excess weight after surgery. Since it brings the lower part of the small intestines directly to the stomach and allows the food to pass directly to this area, it disables a part of the upper small intestines, so its metabolic effects and its effect on diabetes are quite high. The duration of surgery is longer. It requires advanced laparoscopic surgery experience and skill. Although it does not cause vitamin and mineral deficiency, it requires blood test and vitamin/mineral level monitoring at regular intervals.
Transit Bipartition
It is a technique introduced to the medical literature by Brazilian surgeon Sergio Santoro. The Transit Bipartition technique is similar to other techniques, in addition to a sleeve gastrectomy procedure, unlike other procedures, operations on all of the ten parts of the small intestine are performed by providing a second outlet to the lower part of the stomach. In this way, the passage of the eaten food from all segments of the small intestine is ensured.
In Transit Bipartition, first of all, 100 cm is calculated from the point where the small intestines meet with the large intestines and this part is marked. By counting another 150 cm, the small intestine is incised at 250 cm from the junction of the small intestines with the large intestine. The cut lower end is ligated to the stomach. The upper end is ligated to the previously marked 100 cm. In this way, direct food entry is provided to the last 250 cm of the small intestines. The only important point is that approximately 1/3 of the food passes through the duodenum, which is the natural way, and 2/3 passes through the last part of the small intestines thanks to the newly made ligation. The biggest advantage of this surgery is that less than 5% of patients need iron only in the long-term. Since 1/3 of the food passes through the normal digestive tract, more than 95% of patients can continue their lives without the need for any supplements.
Advantages of Transit Bipartition
Less incidence of gastric sleeve leaks due to low intragastric pressure,
Failure of the gastric sleeve to expand due to low pressure in the stomach.
Since the duodenum can be accessed endoscopically, there are no problems with accessing the pancreas and bile ducts.
Continued passage and absorption of food through the entire digestive tract.
Ease of access to all parts of the digestive system endoscopically.
Access to the duodenum and bile ducts for ERCP
Less need for vitamin, mineral, iron and calcium supplements due to the protection of stomach antrum, pylorus and duodenum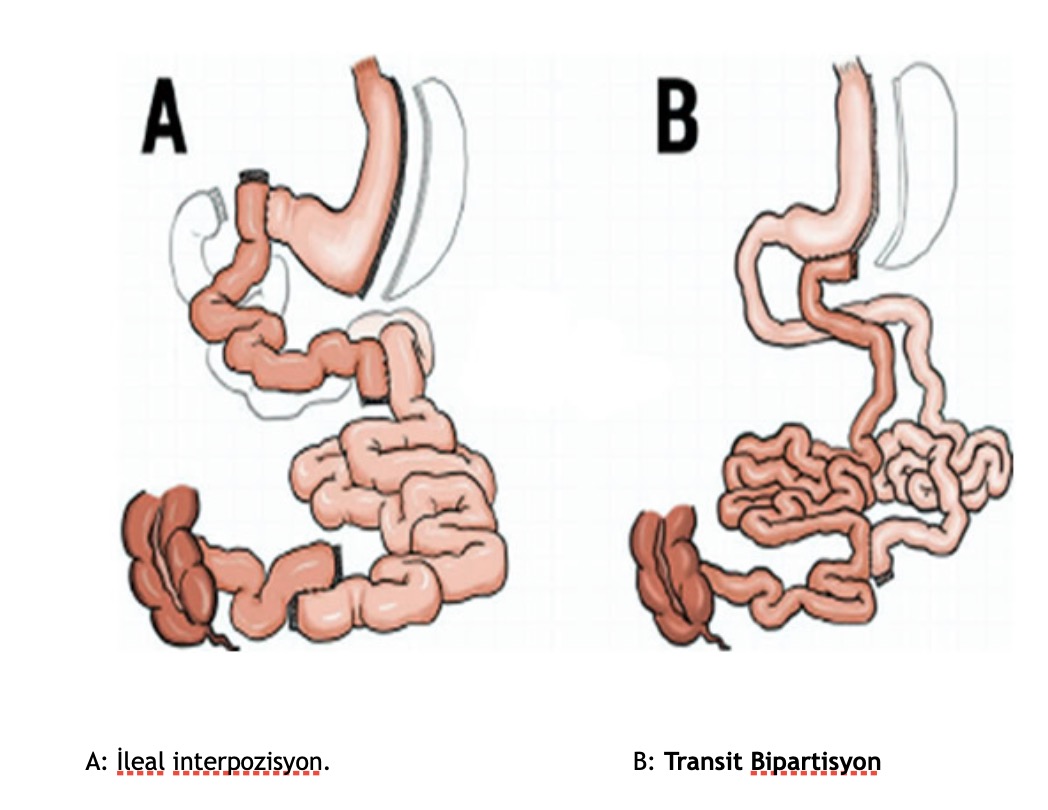
Assoc. Prof. Ahmet Tekin

General Surgeon