ERCP (Endoscopic Retrograde Cholangiopancreatography)
On this page you can find:
* What is ERCP?
* What are the bile and pancreatic ducts?
* When is ERCP performed?
* How is the patient prepared for ERCP?
* How is ERCP performed?
* Laparoscopic cholecystectomy + ERCP (combined operation)
* Post ERCP
* What are the risks of the ERCP operation?
What is ERCP?
Endoscopic retrograde cholangiopancreatography is an operation that combines upper gastrointestinal (GI) endoscopy and x-rays to treat problems of the bile and pancreatic ducts. ERCP is also used to diagnose problems in the bile and pancreatic ducts. However, magnetic resonance cholangiopancreatography (MRCP), a non-invasive method, has replaced ERCP in diagnosis1. For diagnostic purposes, MRCP is first performed. However, if a possible treatment is required following the diagnosis, ERCP is a priority.
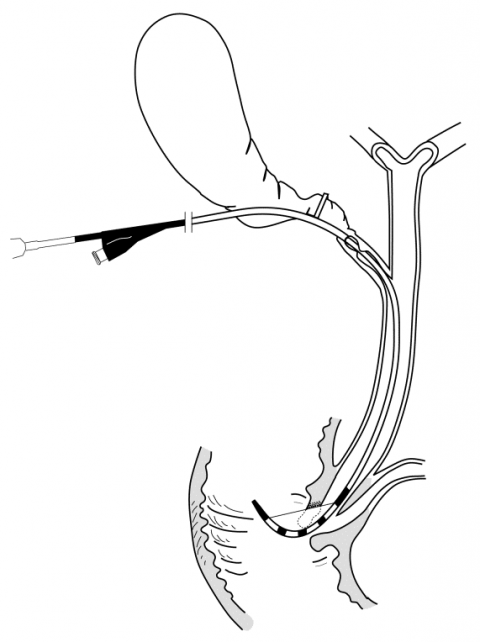
Schematic view of ERCP
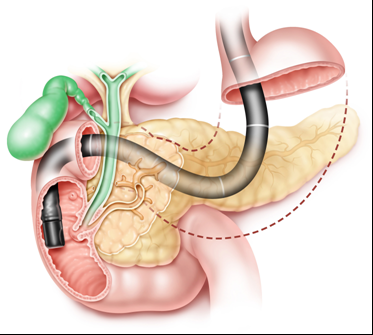
Radiological view of the one-stage operation
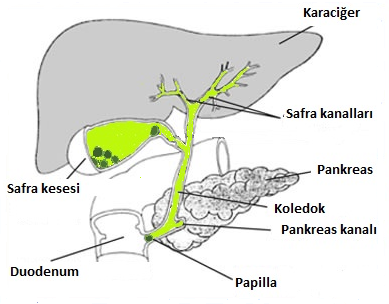
What are the bile and pancreatic ducts?
Bile and pancreatic ducts are fluid-carrying structures in the human body. Bile is created in the liver and flows into the biliary tract via small bile ducts in the liver. Bile ducts store bile and discharge it into the duodenum to aid digestion during meals. Between meals, the distal common bile duct closes and bile is stored in the pear-shaped gallbladder next to the liver. Pancreatic secretion is carried into the main pancreatic duct via small ducts. Pancreatic secretion is carried to the duodenum via the main pancreatic duct, helping to break down food, ie digestion, just like bile. The common bile duct (choledochus) and the main pancreatic duct open into the duodenum through a nipple-shaped projection called papilla. The papilla is 1-1.5 cm in length and its inner lumen diameter is 2-4 mm in width. For this reason, stones larger than 3-4 mm can cause blockage. Since the papilla is in the sphincter structure and contracts while at rest, the pressure in the common bile duct and pancreatic duct is high (20 mmH2O).
Bile ducts carry bile from the liver to the duodenum. The pancreatic duct carries pancreatic fluid to the duodenum.
When is ERCP performed?
ERCP is performed when a narrowing or obstruction occurs in the biliary tract and pancreatic duct due to the following reasons.
* Tumors
* Choledochal stones
* pancreatitis may be traumatic or due to inflammation
* infection
* stenosis of the papillae
* strictures in the ducts called scarring or sclerosis
* pseudocysts that can occur in both ducts
In addition, ERCP is performed for diagnosis and treatment in duct injuries that may occur due to trauma and surgery.
How is the patient prepared for ERCP?
First of all, the patient is informed in detail on the ERCP operation. The upper gastrointestinal tract should be empty. Generally, the patient is not given any food for 8 hours before ERCP. During this period, chewing gum and cigarettes are also prohibited. A detailed history of the patient is requested. Patients should tell the doctor about their current health status, especially if they have heart or lung diseases, diabetes and allergies. Patients should also declare all medications they take. Patients should not take drugs that affect blood coagulation temporarily (antiaggregant-aspirin, anticoagulant-cumadin). These drugs are requested to be discontinued 5 days before the ERCP operation. In addition, drugs that will interact with the tranquilizers given to relax the patient during ERCP should not be taken.
Drugs that should be restricted before and after ERCP:
* non-steroidal anti-inflammatory drugs (aspirin, ibuprofen and naproxen).
* blood thinners (plavix, coumadin)
* high blood pressure medications
* diabetes medications
* antidepressants
* nutritional supplements
It is recommended that patients not drive within 12 hours after ERCP, as they are given sedatives.
How is ERCP performed?
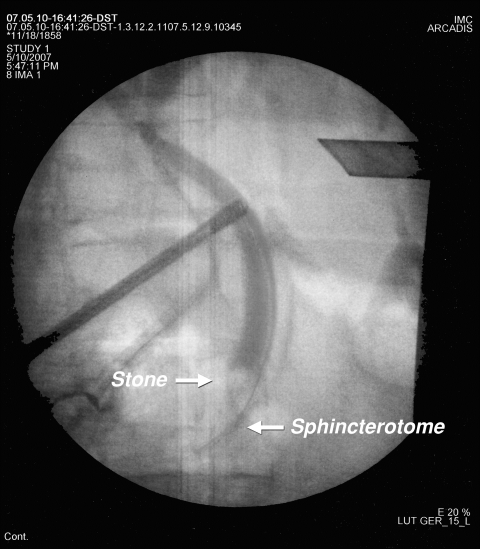
The ERCP operation is performed by gastroenterologists and trained surgeons in a hospital or outpatient center. The throat of the patients is anesthetized with a mouthwash or a spray applied on the back of the throat. Thanks to this local anesthesia, the throat is numbed and the patient's gag reflex is soothed. Vascular access is established for sedatives (tranquilizers) and other drugs to be administered. During the sedation, the vital signs of the patients are monitored by the doctor and other health personnel. In patients who cannot tolerate the procedure with sedatives, it is performed under general anesthesia. During ERCP, patients are placed on the x-ray table on their back or left side. A side-view endoscope (duodenoscope) with a video-camera and light source at the tip is passed through the stomach and inserted into the duodenum. The video-camera transmits the image to a monitor that the doctor and team can watch. Air is pumped through the endoscope into the stomach and duodenum for easy viewing of the image. When the duodenal papilla is seen, a blunt catheter is guided through the papillary opening into the bile duct via the endoscope. After the catheter has passed through the duct within the papilla, a radio-opaque substance is injected through the catheter into the duct. Radio-opaque material, also called contrast material, allows ducts to be seen with x-rays. X-rays allow the diagnosis of many pathologies such as stenosis, obstruction, stone, tumor in the ducts. During the ERCP operation, different treatment procedures can be applied for stenosis and obstruction. During treatment procedures, the doctor uses x-ray video, also called fluoroscopy, to see the ducts. With special tools directed to the ducts through the endoscope, blocked ducts can be opened, gallstones can be removed or broken, a stent can be inserted for tumors. Stents are plastic or expandable metal tubes used to open blocked flow in the bile or pancreatic ducts. A type of biopsy called brush cytology may be done. In this technique, the cells in the ducts are taken for pathological examination by using an appropriate brush through the endoscope. The collected cells are then examined with a microscope for signs of inflammation or cancer. Occasionally, ERCP is performed if surgical bile leakage is suspected after gallbladder surgery. If a biliary tract injury is detected, some types of injury can be treated with a stent or naso-biliary catheter. Laparoscopic cholecystectomy + ERCP (combined operation)
The ERCP operation is most commonly performed for the diagnosis and treatment of bile duct (choledochal) stones. When gallstones + bile duct stones are together, there are different treatment options. 1) First ERCP, then cholecystectomy (removal of the gallbladder), 2) combined operation: cholecystectomy and ERCP performed in the same session 3) first the gallbladder is removed, followed by ERCP and the duct stones are cleared. Today, the most commonly used method is the removal of duct stones with ERCP and cholecystectomy in the follow-up. However, ERCP performed by surgeons and rapid developments in technology have led to the increasing popularity of the single-stage operation (laparoscopic cholecystectomy + ERCP) 2. The one-stage operation has significant advantages over other methods 2,3.
* Both operations are performed in a single session.
* The success rate is higher in ERCP.
* The risk of pancreatitis after ERCP is very low.
* More economical
Due to the above-mentioned advantages, we prefer the single-session operation (lap. Cholecystectomy + ERCP) in patients with gallstones + bile duct stones. The results we have obtained in the single session combined operation technique, which we have been using since 2000, are excellent2,3.
Schematic view of the single-stage operation
Radiological view of the one-stage operation
After ERCP
After ERCP, patients are kept in the recovery room for approximately one hour until the effects of the sedatives wear off. Due to the amnesia effect of sedative drugs, patients may not remember the operation and the post-operational period and the conversations with the health personnel during this period. After ERCP, the patient may feel bloated or nauseous. In addition, patients may have a sore throat that can last for a day or two. The patient can go home within 2-3 hours after the effect of sedative drugs wears off. However, patients should spend the rest of the day resting at home, as they will likely feel tired. Patients can be fed orally 2 hours after the operation and can start taking their medications continuously. ERCP results are reported to the patient immediately after the operation. If a biopsy has been performed, results will be available within a few days.
What are the possible risks of the ERCP operation?
Although ERCP is generally a safe and well-tolerated operation, complications can occur with a frequency of 5-10%, even when performed by an experienced endoscopist.
• Bleeding may occur, especially when the papilla (sphincter) is incised. Bleeding is usually minimal and stops spontaneously. Sometimes blood transfusion may be required. If bleeding occurs during the operation, this can be stopped using a variety of endoscopic techniques, including placement of hemoclips, injection of epinephrine (which constricts blood vessels) or the use of cautery. • Infection (cholangitis), especially in the biliary tract may occur when the bile does not drain well. Some patients may need antibiotics during the operation and for a few days after ERCP. • Pancreatitis (inflammation of the pancreas) occurs in 3% to 5% of all patients undergoing ERCP5. Symptoms such as bloating, belching and severe abdominal pain occur. Pancreatitis after ERCP is usually mild. However, it can be serious and life-threatening, requiring hospitalization in some patients. • Perforation (tear or hole) may occur in the esophagus, stomach, small intestine or bile ducts. While these complications are rare, they are serious complications that are life-threatening when they occur. Urgent surgical repair may be required. • Difficulty in breathing or pneumonia may develop as a result of aspiration. Aspiration occurs as a result of gastric juice or food residues entering the windpipe. This risk is minimized by not giving any food to patients for 3-4 hours before the ERCP operation. • Allergic reactions to sedative and anesthetic drugs may develop.
These complications are usually serious and require hospitalization. If any of the following symptoms occur after ERCP, this is a sign of possible complications and the patient should seek immediate medical attention:
• difficulty swallowing • severe abdominal pain • vomiting • bloody or dark stools • weakness or fainting • fever or chills
Sources
1 Tekin A, Saygili M, Hafta A, Oztan S. Biliary stones and stenoses: diagnostic value of magnetic resonance cholangiography. Turk J Gastroenterol. 2002;13(3):139-45.
2 Tekin A, Ogetman Z, Altunel E, Laparoendoscopic ‘‘rendezvous’’ versus laparoscopic antegrade sphincterotomy for choledocholithiasis. Surgery 2008 ;144:442-7
3 Tekin A, Ogetman Z. Laparoscopic Exploration of the Common Bile Duct with a Rigid Scope in Patients with Problematic Choledocholithiasis. World J Surg. 2010 ;34(8):1894-1897.
4 Andruilli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. American J Gastroenterology. 2007;102:1781–1788.
5 Testoni PA, Mariani A, Giussani A, Vailati C, Masci E, et al.Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterolgy. 2010;105(8):1753-61.
Assoc. Prof. Ahmet Tekin

General Surgeon