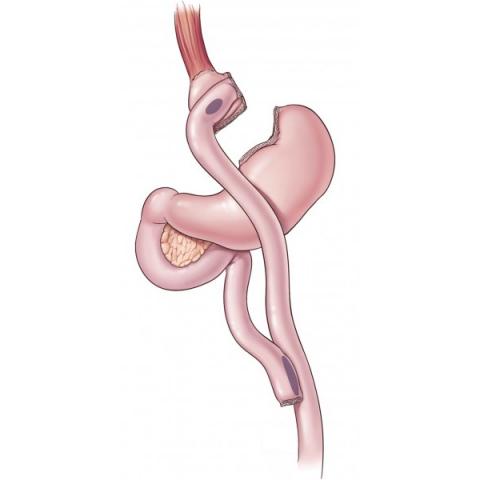
The stomach is divided into 2 separate parts by stapling so that approximately 50-60 ml of volume is left just below the junction of the stomach with the esophagus. Then, a new sac is created between the small intestine and this newly formed stomach sac so that approximately 100 cm of the small intestine is out of digestion. Thus, both the food that the stomach can take will be very limited and the absorption surface of the small intestine will be reduced by about 30%. When the food taken fills the small sac, a feeling of fullness occurs.
It is the most popular and most frequently performed bariatric surgery method. Gastric bypass is an operation that restricts food intake (restrictive) by shrinking the stomach volume and at the same time decreases food absorption (malabsorptive) by disabling the small intestine of 100-150 cm.
Definition
There are two stages of gastric bypass surgery:
At the initial stage, the stomach becomes smaller. A small pouch is created by dividing, with a stapler, the upper part of the stomach close to the esophagus. This pouch is about the size of a tangerine.
The second stage is bypass. The formed gastric sac is connected to the distal of the small intestine (jejunum) with a small hole. The food will go to the small intestine without passing through the duodenum and the first 100-150 cm of the small intestine. Therefore, less of the food will be absorbed, hence fewer calories will be absorbed.
Gastric bypass can be performed with two techniques, open and laparoscopic. Laparoscopic technique is preferred more often. The advantages of laparoscopy over open surgery include:
The shorter the hospitalization period and the faster the recovery.
Less pain.
Smaller scars (4-5 pcs of 0.5-1 cm incisions) and less risk of hernia or infection.
This surgery is performed under general anesthesia and takes about 2 to 3 hours.
Insertion sites for laparoscopic gastric bypass Schematic view of gastric bypass
Who is a candidate for Gastric Bypass?
Morbidly obese patients with a body mass index (BMI-BMI) over 40 are candidates for gastric bypass. Gastric bypass is preferred instead of gastric band and sleeve gastrectomy, especially in obese patients with additional diseases such as type 2 diabetes, hypertension and high cholesterol level. In addition, it can be preferred in super obese patients with BMI ≥ 50.
Obese patients with a BMI between 35 and 40 are candidates for gastric bypass if they have obesity-related diabetes, high blood pressure, high cholesterol, etc.
Risks
Gastric bypass surgery has many risks. Some of these risks are very serious. Detailed information on this matter should be obtained from your doctor.
The main risks associated with surgery and anesthesia are:
Allergic reactions to drugs
Embolism: blood clots that can form in the legs can travel to the lungs.
Bleeding
Difficulty breathing
Heart attack (during or after surgery)
Infection: the surgical site, lung (pneumonia), bladder or kidneys
Leak at the gastric and intestinal anastomosis site
Obstruction of the small intestine
Preoperative preparation
As with other surgical operations, there are pre-operative preparations that must be carried out carefully. Recommendations to you by your doctor are usually as follows.
It is recommended to follow a diet for a week before surgery to reduce the fat around the liver.
Watery food intake for 48 hours before surgery.
In patients with constipation, it is necessary to clean the colon by taking magnesium citrate or Colyte before surgery.
Stop all medications you are taking unless your doctor has advised you to.
If you are using any herbal medicine for headache or allergy or blood thinner, it should be known before the operation.
Stomach endoscopy is usually required before surgery. Gastric hernia, reflux disease, ulcer and tumor should be investigated.
If you smoke, you should stop smoking a few weeks before the surgery. Smoking slows wound healing. It increases the risk of respiratory failure.
Preoperative blood tests and abdominal ultrasonography are performed. Anesthesiology, cardiology and chest diseases consultations may be required to evaluate the risk of operation after the examinations are completed.
After surgery
Postoperative hospital stay is 4-6 days. Patients are usually kept in intensive care units for the first 1 or 2 days.
The patient is mobilized 1 or 2 days after the operation.
A catheter (tube) can be placed in the stomach for 2-3 days.
A bladder catheter can be placed for urination
During the first 3 days it will not be possible to eat. If there is no risk of leakage, watery food is begun to be consumed after the 3rd day and then continues with mashed or soft foods.
A tube can be placed from the nose to the stomach for 2-3 days to empty the stomach contents after the surgery.
Special socks are worn on the feet and legs to help prevent the formation of blood clots.
Medicine (heparin) is administered to prevent blood clots from forming.
Painkillers are given intravenously for pain
The benefits of Gastric Bypass
Most people lose 10 to 15 kg in the first month after surgery. The rate of weight loss will decrease over time. The success rate of losing excess weight after gastric bypass is higher than sleeve gastrectomy. In both methods, food intake is limited. In addition, food absorption is decreased in gastric bypass. Therefore, it is relatively superior to sleeve gastrectomy in losing excess weight.
Within 1 year after the operation, 75% of excess weight is lost. Loss of excess weight reaches 80-90% in the second year. With the loss of excess weight, a significant improvement is also observed in diseases that accompany obesity. A person can regain self-confidence. In addition, with the significant decrease in the load on the knee and waist, most of the knee and low back pain will go away on its own.
RECOVERY RATE FOR OBESITY-RELATED DISEASES (%)
Asthma 82
Gastroesophageal reflux disease (GERD) 90
Hypertension 60-70
High cholesterol level 94
Obstructive sleep apnea 75
Osteoarthritis of the knee and foot joints 85
Type 2 diabetes 70-82
Depression 72
Bypass surgery alone is not a sufficient solution for weight loss. You can get fewer calories with less food. Calorie burn-off should also be increased. This is possible with exercise. In order to prevent complications in the postoperative period, it is necessary to follow the exercise and nutrition rules prescribed by the doctor and dietitian.
There are also risks (complications) seen in the late period after bariatric surgery. These risks are higher after gastric bypass surgery than after sleeve gastrectomy. Vitamin and mineral deficiency is seen in 10-15%. When vitamin and mineral deficiencies are observed in periodic controls, the replacement of vitamin and mineral deficiencies is necessary.
Anemia, vitamin/mineral deficiency, protein malnutrition, temporary hair loss:
Disabling the duodenum and the first part of the small intestine results in decreased absorption of iron and calcium. This condition may cause a predisposition for iron deficiency anemia. Decreased iron absorption can cause severe iron deficiency anemia in female patients with excessive menstrual or hemorrhoidal bleeding.
Women are already at risk for osteoporosis, especially after menopause. Decreased calcium absorption can cause obvious osteoporosis
Chronic anemia may occur due to vitamin B12 deficiencies. The problem is usually treated with vitamin B12 pills or injections.
Known as "dumping syndrome", this condition can occur as a result of rapid emptying of stomach contents into the small intestine. It is triggered by consuming large amounts of food, such as too much sugar or sweets. Although it is not considered a serious risk to general health, it can sometimes be extremely uncomfortable and can cause nausea, weakness, sweating, fainting, etc. after a meal. Some patients cannot tolerate sweets after surgery.
Gallstones may develop following the rapid weight loss of patients.
Alternative Names
Bariatric Surgery - gastric bypass – stomach bypass - Roux-en-Y gastric bypass;